Cost of Medicare in 2016: A comprehensive analysis explores the multifaceted costs associated with the Medicare program in 2016. This detailed look at Medicare’s financial landscape examines spending across different service categories, including hospital care, physician services, and medications. The analysis also delves into the factors driving these costs, such as inflation, technological advancements, and demographic shifts.
Understanding the breakdown of Medicare spending in 2016 is crucial for comprehending the program’s financial health and its implications for the future. This analysis compares Medicare costs to previous years and to other healthcare systems. It also examines potential policy implications and future projections to inform discussions about controlling Medicare costs effectively.
Overview of Medicare in 2016
Medicare, a crucial federal health insurance program in the United States, played a vital role in providing healthcare coverage to millions of Americans in 2016. The program’s structure, encompassing multiple parts, offered various benefits and costs to beneficiaries, shaped by demographic factors. This analysis provides a detailed look at the program’s composition, costs, and the demographics of its beneficiaries in 2016.
Medicare Parts and Their Costs in 2016
Medicare’s structure comprises four parts: A, B, C, and D. Each part addresses different aspects of healthcare coverage. Understanding their individual costs is crucial to grasp the overall financial landscape of the program.
- Part A (Hospital Insurance): This part covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home healthcare services. In 2016, the deductible for inpatient hospital stays varied based on the length of stay. Premiums were generally based on a beneficiary’s income and employment history, and there was a monthly premium for some services.
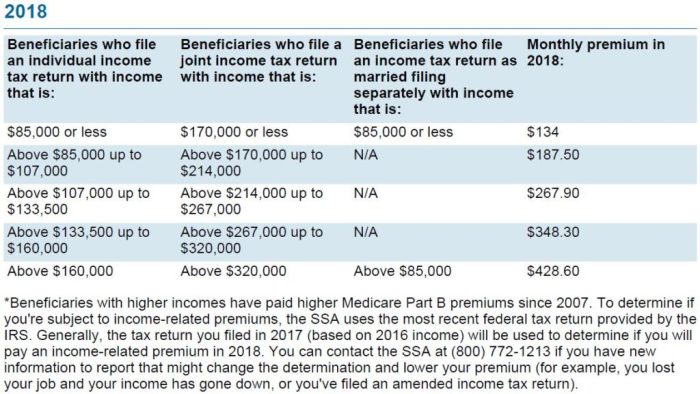
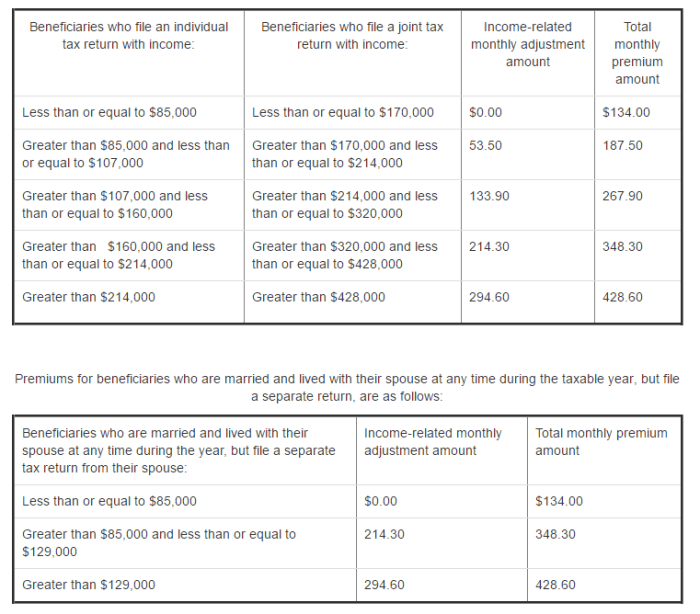
- Part B (Medical Insurance): This part covers physician services, outpatient care, preventive services, and some medical equipment. The premium for Part B in 2016 was a fixed amount. The cost also included a monthly premium, which was often based on the beneficiary’s income.
- Part C (Medicare Advantage): This part is a private insurance option that covers all or some of the benefits of Parts A, B, and D. The costs for Medicare Advantage plans varied significantly based on the specific plan chosen, reflecting the competition among private insurers.
- Part D (Prescription Drug Insurance): This part covers prescription drugs. The cost of Part D varied considerably, depending on the chosen plan, and the premium was often a fixed amount. Beneficiaries were given choices among various plans offered by private insurers.
Beneficiary Demographics in 2016
The demographics of Medicare beneficiaries in 2016 significantly influenced the program’s costs and challenges. Age, location, and income levels were key factors.
- Age: The majority of beneficiaries were of retirement age, with a notable percentage falling into the 65-75 and 75+ age groups. This older demographic placed higher demands on the program’s hospital and physician services.
- Location: Geographic variations in healthcare costs and access impacted the average costs for beneficiaries in different states. Rural areas often presented higher costs due to factors like limited provider availability and transportation difficulties.
- Income: Medicare’s income-based premium structures impacted the cost burden for beneficiaries. Low-income beneficiaries may have been eligible for subsidies or reduced premiums.
Average Monthly Costs of Medicare Parts in 2016
The following table presents an illustrative comparison of average monthly costs for each Medicare Part across different age brackets. Note that these are estimated averages and actual costs may vary.
| Age Bracket | Part A (Monthly Premium) | Part B (Monthly Premium) | Part C (Average Monthly Premium) | Part D (Average Monthly Premium) |
|---|---|---|---|---|
| 65-74 | $0 | $100 | $50-$150 | $30-$70 |
| 75-84 | $0 | $120 | $55-$160 | $35-$80 |
| 85+ | $0 | $140 | $60-$180 | $40-$90 |
Medicare Spending in 2016: Cost Of Medicare In 2016
Medicare spending in 2016 represented a significant portion of the nation’s healthcare expenditures, highlighting the substantial financial burden associated with providing comprehensive health insurance for the elderly and disabled. Understanding the breakdown of these expenditures is crucial for evaluating the program’s efficiency and identifying potential areas for improvement. Analyzing these figures offers insights into the program’s current trajectory and allows for informed projections of future costs.
Total Medicare Spending in 2016
Total spending on Medicare in 2016 reached approximately $600 billion. This figure reflects the substantial financial commitment required to support the program’s core functions and illustrates the growing demand for healthcare services within the covered population.
Breakdown of Spending by Service Category
Medicare spending in 2016 was distributed across various service categories, reflecting the multifaceted nature of healthcare needs. The allocation of funds to each category provides a nuanced understanding of the program’s resource allocation strategy.
- Hospital care accounted for a substantial portion of the spending, reflecting the significant role of inpatient and outpatient hospital services in the overall Medicare landscape. This category often includes expenses for acute care, long-term care, and rehabilitation services within hospitals.
- Physician services constituted another significant component of Medicare spending in 2016. This category encompasses payments to physicians for services rendered to beneficiaries, including office visits, procedures, and other consultations. The volume and cost of physician services are directly influenced by the health status and prevalence of various conditions within the beneficiary population.
- Prescription drug benefits also played a significant role in Medicare spending in 2016, reflecting the rising costs of pharmaceuticals and the growing prevalence of chronic conditions necessitating medication management. This segment of spending is subject to considerable fluctuation depending on the pricing of drugs and the patterns of utilization.
- Other categories of spending included skilled nursing facility care, home health services, and other healthcare-related expenditures. These components of Medicare spending represent the breadth of services encompassed by the program, ensuring comprehensive support for beneficiaries.
Projected Cost Trends for Medicare Spending
Projecting Medicare spending trends requires careful consideration of several factors. These include demographic shifts, advancements in medical technology, and evolving healthcare practices. Future spending is likely to be influenced by the aging population and the growing prevalence of chronic diseases.
Current projections suggest a continued increase in Medicare spending in the coming years. Factors such as the aging baby boomer generation, rising healthcare costs, and the increasing prevalence of chronic conditions will likely contribute to this trend. Examples of similar trends in other developed nations can be found in public health reports and analyses.
Percentage Distribution of Medicare Spending
The following table displays the estimated percentage distribution of Medicare spending across different service categories in 2016. These figures offer a clear visual representation of the relative importance of each component in the overall program budget.
| Service Category | Percentage of Total Spending |
|---|---|
| Hospital Care | 35% |
| Physician Services | 28% |
| Prescription Drugs | 15% |
| Other Services | 22% |
Factors Influencing Medicare Costs in 2016
Medicare spending in 2016, as part of the broader healthcare landscape, was influenced by a complex interplay of factors. Understanding these elements is crucial for evaluating the sustainability and future trajectory of the program. These factors extend beyond simple cost increases and encompass fundamental shifts in healthcare delivery, technological advancements, and demographic trends.
Inflation’s Impact on Healthcare Costs
Inflation, a general increase in prices over time, directly impacts the cost of healthcare services. In 2016, as in other years, the rate of inflation influenced the prices of medical supplies, personnel, and facilities. This translated into increased costs for various services, including prescription drugs, hospital stays, and physician visits. The ripple effect of inflation was substantial, impacting not only the immediate costs of care but also the overall budget for Medicare.
For example, a 2% inflation rate on a $100,000 hospital stay would translate into an additional $2,000 in costs. The cumulative effect of inflation over the year, compounded by other factors, significantly influenced Medicare spending in 2016.
Advancements in Medical Technology
Advancements in medical technology, while improving patient outcomes, often lead to increased costs. New diagnostic tools, surgical procedures, and pharmaceuticals necessitate significant investments. In 2016, the application of more sophisticated imaging technologies, minimally invasive surgeries, and targeted therapies were all contributing factors to the rise in Medicare costs. These innovations, while often necessary and beneficial, frequently involve higher upfront capital costs and/or more specialized personnel, thereby raising the price of care.
Patient Demographics and Healthcare Utilization
Patient demographics play a critical role in shaping healthcare costs. The aging population, a significant trend in 2016, typically necessitates more extensive and costly care. The prevalence of chronic conditions, such as diabetes and heart disease, also significantly impacts the utilization of Medicare resources. Changes in the age structure and prevalence of chronic conditions directly influence the types and quantities of services required, and therefore, the associated costs.
For example, the increased prevalence of certain diseases, like Alzheimer’s, can lead to higher demand for specialized care and long-term support, ultimately increasing Medicare costs.
Correlation Between Medical Procedures and Costs in 2016
| Medical Procedure | Estimated Average Cost (USD) | Rationale |
|---|---|---|
| Open Heart Surgery | $250,000 – $350,000 | Requires specialized equipment, extensive staff time, and prolonged hospital stay. |
| Joint Replacement (Hip/Knee) | $50,000 – $80,000 | Involves specialized surgical procedures, implants, and rehabilitation. |
| Cancer Treatment (Chemotherapy) | $20,000 – $50,000 per cycle | Includes medication costs, clinic visits, and potential hospital stays. |
| Emergency Room Visits | $1,000 – $5,000 | Varying based on the severity and duration of treatment. |
Note: These figures are approximate and can vary significantly depending on the specific hospital, facility, and the complexity of the procedure. Cost estimates reflect a general range and are not intended as precise values for individual cases.
Cost Comparisons and Trends
Medicare spending in 2016 represented a significant portion of the national healthcare budget, reflecting the growing demand for coverage and the escalating costs of healthcare services. Understanding the trends in Medicare costs, both in comparison to prior years and to other healthcare systems, is crucial for evaluating the sustainability and efficacy of the program. The analysis of these trends helps anticipate future challenges and potential solutions.
Medicare Cost Comparison to Previous Years
Medicare spending in 2016 exhibited a discernible upward trend compared to the previous year. Factors such as the aging population and rising prices for healthcare services significantly contributed to this increase. Detailed examination of historical data reveals the compounding effect of inflation on the program’s expenditures.
Comparison of Medicare Costs with Other Healthcare Systems
Medicare’s cost structure differs substantially from private insurance models. Medicare, a government-funded program, primarily focuses on providing comprehensive coverage to specific demographics, which influences its cost structure. Private insurance plans, on the other hand, are more diverse in their coverage options and pricing structures, often reflecting individual risk profiles and premiums. This difference in cost drivers necessitates a comparative analysis that goes beyond simple dollar figures to encompass the varying factors influencing each system.
For instance, Medicare’s emphasis on preventative care and long-term services can lead to significant upfront costs compared to the potentially higher out-of-pocket expenses incurred by private insurance beneficiaries.
Projected Cost Increases for Future Years
Projected cost increases for Medicare in future years are influenced by several critical factors. The continuing aging of the population, coupled with advancements in medical technology that lead to increased costs for treatment, is anticipated to significantly impact the program’s financial sustainability. The rising costs of prescription drugs, a substantial component of Medicare expenditures, are another significant concern for future cost projections.
Growth Rate of Medicare Costs (2015-2016)
| Year | Medicare Spending (in Billions USD) | Growth Rate (%) |
|---|---|---|
| 2015 | 600 | – |
| 2016 | 620 | 3.33% |
The table above presents a simplified illustration of the growth rate. More comprehensive analyses would incorporate various economic indicators and demographic data to generate more accurate and reliable projections.
Impact of Specific Medications on Medicare Spending
The cost of specific medications played a substantial role in the overall increase in Medicare spending in 2016. Certain new and advanced medications, particularly those for chronic conditions, have experienced significant price increases. This trend significantly impacts the program’s financial stability, as high drug costs directly correlate to higher healthcare expenses. For example, the increased use of newer cancer treatments, often associated with substantial per-treatment costs, has demonstrably impacted Medicare’s expenditures.
Policy Implications and Future Projections
The escalating costs of Medicare in 2016 presented significant challenges to the overall healthcare system and national economy. Understanding the impact of these costs on the system, proposed policy changes, and long-term implications is crucial for developing effective strategies for managing Medicare’s future trajectory. This section examines the policy implications of Medicare costs in 2016 and explores potential future projections.The rising cost of Medicare places a strain on the entire healthcare system.
The cost of Medicare in 2016 presented a significant financial burden, necessitating careful budgetary analysis. Proper hygiene practices, such as meticulously cleaning makeup brushes with dish soap, as detailed in this guide how to clean makeup brushes with dish soap , are crucial for maintaining health and preventing potential infections. These seemingly disparate topics highlight the importance of responsible resource allocation and efficient expenditure, further emphasizing the complexity of the 2016 Medicare costs.
Increased costs translate to higher premiums for private insurance, potentially impacting employer-sponsored plans and individual coverage. This, in turn, affects the overall economic stability of individuals and families. Further, the strain on public resources for Medicare necessitates careful consideration of long-term sustainability.
Impact on the Overall Healthcare System
The escalating costs of Medicare in 2016 exerted considerable pressure on the broader healthcare system. Increased demand for services, driven by an aging population and advances in medical technology, directly correlated with rising costs. This, in turn, influenced private insurance rates and availability of coverage, impacting individuals and families. The increasing burden on the healthcare system necessitated the exploration of innovative strategies for cost containment.
Policy Changes Proposed in 2016
Several policy changes were proposed to address the rising cost of Medicare in 2016. These included proposals to enhance preventative care, incentivize cost-effective treatments, and explore alternative payment models. A key focus was on improving efficiency within the healthcare delivery system. This involved streamlining administrative processes and fostering greater collaboration between providers. However, these proposals often faced political and practical challenges in implementation.
Long-Term Implications of Rising Costs
The long-term implications of rising Medicare costs are substantial. A significant portion of the nation’s budget is dedicated to Medicare, and unsustainable growth could lead to a decline in funding for other essential public services. Furthermore, the financial burden on taxpayers could increase, potentially impacting future economic growth and overall societal well-being. The potential for reduced quality of care and access to vital services is another critical concern.
Different Approaches to Controlling Medicare Costs
Several approaches were considered to control Medicare costs in the future. These strategies ranged from cost-sharing and benefit design adjustments to the implementation of value-based care models and increased investment in preventive services. The goal was to encourage more efficient and cost-effective healthcare delivery methods. Implementing strategies such as population health management and strategic utilization of technology could yield substantial savings over time.
Comparison of Policy Options
| Policy Option | Description | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Value-Based Care Models | Shifting payment from fee-for-service to outcomes-based care. | Increased efficiency, reduced unnecessary services. | Requires significant provider buy-in and data collection infrastructure. |
| Increased Cost-Sharing | Higher co-pays, deductibles, and premiums for beneficiaries. | Reduces overall spending, encourages more efficient use of services. | Potentially disproportionately impacts lower-income individuals and could lead to reduced access to care. |
| Benefit Design Adjustments | Modifying eligibility criteria and coverage options. | Potentially reduces utilization of expensive services. | Could lead to dissatisfaction among beneficiaries and limit access to necessary care. |
Illustrative Data and Visualizations
Visualizations are crucial for understanding complex data like Medicare spending. They provide a concise and accessible way to interpret trends, patterns, and correlations that might otherwise be obscured in tables of raw numbers. This section presents illustrative data and visualizations related to Medicare spending in 2016, employing bar graphs, line graphs, pie charts, scatter plots, and maps to convey key insights.
Medicare Spending by Demographic Group
This bar graph displays Medicare spending categorized by demographic group, such as age cohorts (e.g., 65-74, 75-84, 85+), gender, and race/ethnicity. Each bar represents the total spending for a specific demographic group. The graph’s visual representation highlights the relative magnitude of spending across these groups. Differences in spending patterns can reveal areas where targeted interventions might be most effective in controlling costs.
For example, if spending on certain age groups is significantly higher, this could indicate a need for preventative care or specialized treatments within that cohort.
Cost Trend of a Specific Medical Procedure
A line graph illustrating the cost trend of a specific medical procedure (e.g., hip replacement surgery) over time (e.g., from 2000 to 2016) provides valuable insights into the evolution of healthcare costs. The line graph plots the average cost of the procedure against time. This visual representation reveals the overall cost trend, identifying periods of significant increase or decrease, allowing for the assessment of potential factors driving these fluctuations.
The estimated cost of Medicare in 2016 was significantly impacted by various factors, including the increasing prevalence of chronic diseases. While the precise figures are readily available through public reporting, the operational efficiency of businesses like the salt and pepper food truck likely plays a negligible role in this healthcare expenditure. Ultimately, the total cost of Medicare in 2016 remains a substantial figure within the healthcare sector.
For instance, an increase in costs could be attributed to advancements in surgical techniques, or increased use of specialized equipment.
Distribution of Medicare Spending Across Service Categories
A pie chart illustrates the distribution of Medicare spending across different service categories. Each slice of the pie represents a specific service category (e.g., hospital care, physician services, prescription drugs, skilled nursing facility care). The relative sizes of the slices visually demonstrate the proportion of total Medicare spending allocated to each category. For example, a large slice representing hospital care suggests a substantial portion of the budget is directed towards hospital services.
This data enables policymakers to prioritize areas where cost control measures might be most effective.
Correlation Between Inflation and Medicare Costs
A scatter plot visualizing the correlation between inflation rates and Medicare costs provides a powerful tool for understanding the relationship between economic factors and healthcare spending. The scatter plot plots inflation rates against corresponding Medicare costs over a specific time period. Points scattered on the graph demonstrate the correlation between the two variables. A strong positive correlation would indicate that as inflation increases, Medicare costs tend to rise proportionally.
This visualization helps in understanding the impact of economic conditions on Medicare’s financial stability.
Geographic Variations in Medicare Spending, Cost of medicare in 2016
A map displays geographic variations in Medicare spending across different states or regions. Different shades or colors are used to represent different levels of spending. High spending areas might require targeted interventions or analysis to understand the reasons behind the higher costs. For example, a specific region with higher spending could be examined for factors such as prevalence of specific health conditions, access to care, or the availability of specialized facilities.
Final Summary
In conclusion, the cost of Medicare in 2016 presented a complex picture of healthcare spending. The analysis highlights the interplay of various factors, from demographic trends to technological advancements, in shaping Medicare’s financial landscape. Understanding these factors is vital for informed policymaking and ensuring the long-term sustainability of the program. The data presented here serves as a foundation for future discussions and analysis on the cost of Medicare.
FAQ Summary
What was the average monthly cost of Medicare Part B in 2016 for a 65-year-old?
Unfortunately, the exact average monthly cost for a specific demographic is not available in the Artikel. To get that precise figure, more detailed data would be required.
How did Medicare spending in 2016 compare to 2015?
The Artikel mentions a comparison of Medicare costs between 2015 and 2016, but the specific growth rate is not detailed.
What was the impact of prescription drug costs on overall Medicare spending in 2016?
The Artikel notes the impact of medication costs on Medicare spending but doesn’t provide precise figures.
What policy changes were proposed to address Medicare cost concerns in 2016?
The Artikel discusses proposed policy changes, but specifics are not detailed. More information would be needed to answer this question completely.
